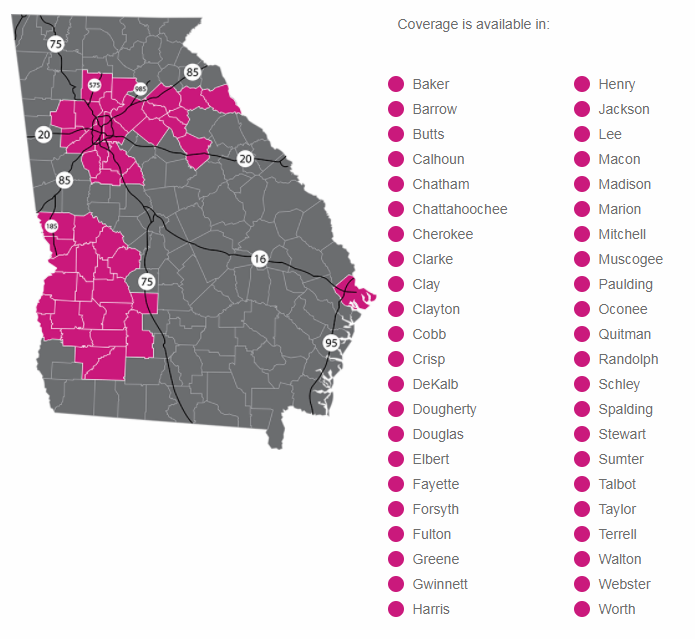
The Individual Health Insurance Market in Georgia continues to have limited plans available. They are HMO’s only; Ambetter, Kaiser and BlueCross is available in 74 Georgia counties including the Atlanta metro.
Recent News Release: Ambetter has just added Piedmont Hospital of Atlanta to their network. Ambetter is in the process of contracting with Piedmont doctors. Our experience is that most Piedmont doctors and doctor groups will join, some will not. Please use the “Find a Doctor” online search tool on our 2019 Recommended Plans page or check with your doctor’s office.
They also have most of the other Piedmont hospital locations.
BlueCross is a Gatekeeper HMO in the nine county Atlanta metro areas. It requires members to select a PCP (Primary Care Physician) within 30 days of enrollment and the PCP acts as a gatekeeper to specialists; the PCP is responsible to get the HMO’s approval for the member to see an In-network specialist. If the BC member goes directly to a BC HMO specialist, there is no coverage. Member pays all costs.
Ambetter is a Non-Gatekeeper HMO. Members can schedule appointments at will directly to see specialists.
BlueCross HMO outside of Atlanta metro is not a gatekeeper; member can schedule appointments direct with specialists.
The 2019 BC HMO Bronze level high deductible HSA plans will be lower cost than Ambetter. The 2019 BC HMO Silver level plans are priced similar to Ambetters’ Silver plans.
Ambetter has the best Gold level plan – it’s actually reasonably price…. relatively speaking. Kaiser will be more expensive in most cases.
The primary differences between Ambetter and BlueCross’s Hospital Network: Ambetter has Emory Health Care System and Piedmont Hospital, BlueCross does not.
BlueCross has Northside Health Care System, Ambetter does not. They both have Wellstar, DeKalb, and Gwinnett.
The Ambetter and BlueCross plans are similar for 2019. The client’s choice will likely be driven by the Networks. We have network comparison tools on our 2019 Recommended Plans web page.
With all HMO plans there is no coverage or benefits when seeing an out of network provider unless it is a true emergency.
Clients currently on a 2018 Ambetter or Kaiser plan will automatically renew at the new rate provided in their renewal letter from their insurance company. No action is required.
If a client is receiving a 2018 subsidy and their estimated income for 2019 will be different than reported for 2018 – by more than just a few thousand dollars – contact our office for updating.
We have received mostly positive feedback from our several hundred Ambetter clients, especially those using the Emory Health Care System.
What’s the Strategy for 2019?
- Choose from the HMO plans available:
- Try to use an In-network PCP for healthy check-ups. Most of the preventative care expenses will be covered at 100% with no deductible for the member.
- If trying to get an expensive medication approved, be ready to ask your current/previous doctor to forward records of failed attempts at step therapy with lower cost medications.
- Know you can still see your current doctor; ask for the private pay (reduced) fee schedule.
- Consider a Health Saving Account with the HMO plan. HSA (pre-tax saving) can be used to pay for medical expenses for care outside the HMO network.
- Clients without pre-existing conditions may want to consider a new One Year PPO Plan with Look for the button on our home page. A pre-existing condition is usually defined as anything the individual has been treated for, consulted a doctor for or taken medication for in the previous 24 months. Pre-existing conditions are not covered. These plans do have large national networks (including Piedmont and Emory) and cost approximately 50% less than the Obamacare HMOs. Be careful and think through the effect of the pre-existing exclusion. Our reps can help with this.
- We encourage clients to see if a Group Health Plan might They still offer the large national networks, richer benefits, tax advantages, and slightly lower cost.
Joe LePage